“I am a nurse.”
This is the answer to the question, “What do you do for a living?”
It is the response given when asked why you know so much about cardiac rhythms, or the flu, or how you can talk about copious bodily fluids the same way someone might talk about their favorite sweater.
It is also the reason why a child’s persistent cough at the playground or an elderly neighbor’s shortness of breath while retrieving their newspaper sets your attention on edge, discreetly looking for pallor and retractions.
Being a nurse is not just your profession, it is encoded in your DNA. The nursing process is now compulsory, as your brain exists in a continuous cycle of assessment to evaluation, transformed from conscious thinking to intuition. You can’t not do it. It is who you are, what you breathe, and how you speak.
Am I (still) a nurse?
When nursing professional development (NPD) practitioners are asked, “What do you do for work?” our response often begins with, “Well, I used to be an ICU nurse, but now I work in nursing professional development, which means I…,” our voices trailing off in response to a puzzled listener’s expression. We speak as though creating an immediate tie to patient care is the only validation for our professional identity as a nurse. “When I took care of patients” can feel like a necessary justification to why we identify as a nurse even though we may no longer routinely don gloves or pass meds. And because many people outside of nursing have a narrow understanding of who a nurse is and what they do, we attempt to validate our identity for them.
Godfrey & Young (2021, p. 363) define professional identity in nursing as “a sense of oneself, and in relationship with others, that is influenced by characteristics, norms, and values of the nursing discipline, resulting in an individual thinking, acting, and feeling like a nurse.” A desire to link who we are as NPD practitioners to who we were as patient care-providing clinicians is legitimized when we consider that the majority of our nursing professional identity forms in our inaugural years as nurses (Priddy et al., 2020). Our field has long known that new nurses embody their professional identity as “doing” (Crigger & Godfrey, 2011; Duchscher, 2008), and more specifically, doing for, around, or to a patient we are caring for. So, when we aren’t performing the traditional patient care tasks of a nurse often (or at all), disconnection from “being” a nurse can result.
I really am a nurse.
Professional identity begins to change when a nurse moves into a leadership or advanced practice role, when their new role and resulting knowledge deficit disrupts their sense of professional self (Priddy et al., 2020). While NPD practitioners may not hold formal leadership titles in their organizations, all function in a leader role within the NPD specialty responsibilities (Harper & Maloney, 2022). Kauffman & Aucoin (2021) describe lack of role clarity as a challenge for nurses transitioning to leadership roles, and NPD practitioners may resonate with this experience. If challenges such as unclear roles continue, the impact on professional identity may be hard for NPD practitioners to overcome.
Colleagues in nursing academia describe a comparable identity disruption when moving from the bedside to the classroom, but also describe a reclaiming of identity rooted in their role’s potential for meaningful impact (Brower et al., 2022). Finding meaning in work, having a sense of professional contribution, and sharing knowledge with colleagues have been demonstrated to increase a sense of belonging to the nursing profession and increase professional identity, contributing to a resolve to remain in the nursing profession (Kristoffersen, 2020).
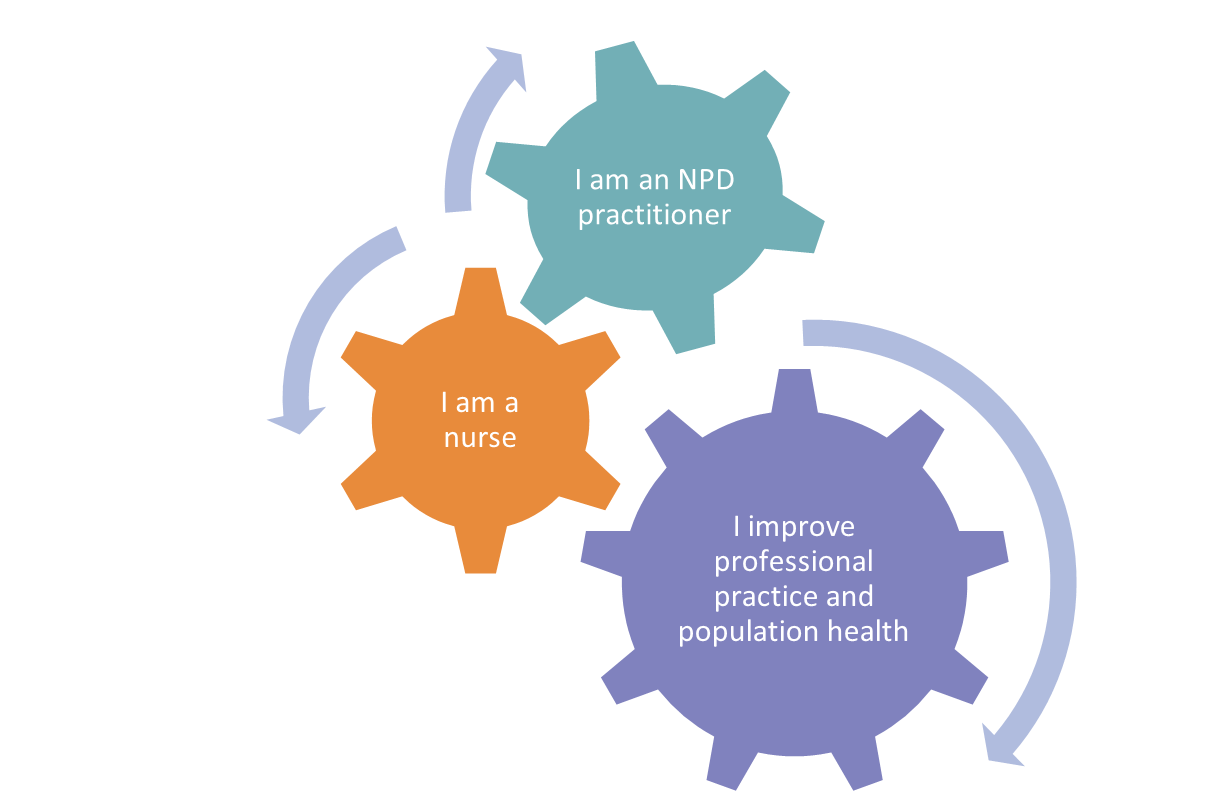
The American Nurses Association (ANA) recognizes that a clearly described nursing specialty practice allows other nurses and the public “to gain familiarity and understanding of the nursing specialty and its contribution to nursing and health care” (American Nurses Association, 2017, p. 12). Nursing professional development, an ANA-recognized nursing specialty, is defined as “a nursing practice specialty that improves the professional practice and role competence of nurses and other healthcare personnel by facilitating ongoing learning, change, and role competence and growth with the intention of improving population health through indirect care” (Harper & Maloney, 2022, p. 16). Reflecting on this definition and the NPD Practice Model, our contribution is twofold. We positively impact the nursing profession by our work with care-providing nurses. And we contribute to population health care by influencing the care provided.
I am a nurse, and so are you.
Every moment of your nursing practice has contributed to forming your nursing professional identity. To those experiences, NPD practitioners add new skills with exponential impact on both health care professionals and the people they provide care for. Our nursing care is reframed from direct patient care delivery to operationalizing caring science into every aspect of our NPD practice (Martin, 2015). Our nursing identity encompasses more than our former direct-care nursing specialty, and we can simultaneously honor our nursing roots while recognizing the power and impact of our NPD specialty.
The American Nurses Association (2021) identifies professional identity growth as the ability to be flexible and change our self-perception over the course of our careers. We change specialties, sometimes multiple times. We have unexpected life events that impact our careers. We retire to enjoy our latter years and continue to give to the next generation of nurses freely through volunteering and mentoring. Flexibility allows us to move through these transitions without losing ourselves.
You are not the nurse you were at the beginning of your career. You are part of an emboldened community of nurses who ensure clinicians have the knowledge, skills, and attitude to provide excellent care. You are a nurse who positively impacts nurses and other clinicians, and ultimately contribute to the improvement of health outcomes. You are a nurse, and so am I. We are NPD practitioners.
References
American Nurses Association. (2017). American Nurses Association recognition of a nursing specialty, approval of a specialty scope of practice statement, acknowledgement of specialty nursing standards of practice, and affirmation of focused practice competencies. https://www.nursingworld.org/~4989de/globalassets/practiceandpolicy/scope-of-practice/3sc-booklet-final-2017-08-17.pdf
American Nurses Association. (2021). Nursing: Scope and standards of practice. (4th ed.). American Nurses Association.
Brower, E., Nemec, R., Ritchie, H., & Nicastro, O. (2022). A qualitative exploration of self-identity during the role transition to a nurse educator. Nurse Education Today, 112. https://doi.org/10.1016/j.nedt.2022.105331
Crigger, N., & Godfrey, N. (2011). The making of nurse professionals: A transformational, ethical approach. Jones & Bartlett.
Duchscher, J. B. (2008). A process of becoming: The stages of new nursing graduate professional role transition. Journal of Continuing Education in Nursing, 39(10), 441-450. doi: 10.3928/00220124-20081001-03
Godfrey, N., & Young, E. (2021). Professional identity. In J. Giddens (Ed.), Concepts of nursing practice (3rd ed.), p. 363-370. Elsevier.
Harper, M. G., & Maloney, P. (Eds.). (2022). Nursing professional development: Scope and standards of practice (4th Ed.). Association for Nursing Professional Development.
Kauffman, S. R., & Aucoin, J. W. (2021). Building a transition program for senior nurse leaders. Journal for Nurses in Professional Development, (39)1, 12-17. DOI: 10.1097/NND.0000000000000781
Kristoffersen, M. (2021). Does professional identity play a critical role in the choice to remain in the nursing profession? Nursing Open, 8(4), 1928-1936. DOI: 10.1002/nop2.862
Martin, M. B. (2015). Caring in nursing professional development. Journal for Nurses in Professional Development, 31(5), 271-277. DOI: 10.1097/NND.0000000000000172
Priddy, K. D., Read, J. L., & Weybrew, K. (2020). Professional identity in nursing: Background & introduction [Video]. Sigma Repository. https://sigma.nursingrepository.org/handle/10755/21082
Mary Smith, MSN, RN, NPD-BC, NC-BC, AMB-BC, C-EFM, CCE
NPD Education Program Manager, ANPD
Mary Smith is ANPD’s NPD education program manager. Leveraging 25 years of experience as a registered nurse and a graduate education in nursing, Mary is committed to serving the needs of the ANPD community. Mary is a published author and a national nursing publication peer reviewer, fostering the support of continued professional development and growth of nurses. She has experience spanning inpatient and outpatient work in obstetrical nursing, regulatory and nursing leadership, and as a nurse coach, which have provided a broad foundation for her continued work in nursing professional development with ANPD.