Nursing professional development (NPD) practitioners understand the inconsistencies in available resources at various healthcare settings. Educational programs designed for the broader hospital system nursing departments may not provide the specialized training required for equipment used in ambulatory settings. This challenges organizations encompassing a wide range of healthcare environments to ensure all staff receive the appropriate education and possess the necessary skills to excel in their specific roles.
At the 2024 ANPD Aspire Convention, Sydney Bush-Foster, MSN, RN, NPD-BC, and Suzanne Duckworth, MSN, RN, AMB-BC, presented a session titled "Ambulatory Mock Code: Making Mock Code Meaningful for Multiple Locations." They shared their experience of identifying the need for more comprehensive mock code education in ambulatory settings and their innovative approach to delivering this training in an engaging and successful manner.
Discovering a Gap
Bush-Foster and Duckworth noticed a recurring issue: clinic managers frequently requested additional support for staff struggling with code responses after the completion of the competency check-off season. To address these concerns, Bush-Foster and Duckworth’s team collaborated with clinic managers and leaders. Discussions revealed mock code training as a key area for improvement.
Previously, all staff were required to have BLS (licensed) and BLS or Heartsaver CPR training (non-licensed). The every two-year mock code competency mirrored a hospital system model, relying heavily on hospital equipment like crash carts, in wall oxygen and suction. This approach, however, didn't account for the diverse staff and equipment variations across their 200+ ambulatory centers. The existing hospital-focused training wasn't preparing staff for real-world code situations in ambulatory settings.
Hospital environments offer the potential for early recognition, prevention, and rapid response to patient deterioration. Dedicated rapid response teams can typically arrive within minutes, significantly increasing the chances of a successful outcome. In contrast, ambulatory settings lack these advantages. Early detection of patient decline can be more challenging, and there are no rapid response teams or overhead paging systems to mobilize assistance. Perhaps the most significant disparity lies in emergency team response times. While in-patient settings benefit from proximity to emergency personnel, ambulatory settings may experience delays of 15 to 20 minutes waiting for Emergency Medical Services to arrive.
Building a Program for Unique Needs
When Bush-Foster and Duckworth recognized their existing in-patient-focused mock code training wasn't meeting the needs of their licensed and non-licensed ambulatory staff, they created a plan for change.
The first step was to assemble a team with expertise across various disciplines. This enterprise-wide competency team included nurses, pharmacists, clinic leaders, response teams, and the medical team. All contributed valuable insights. This collaboration identified critical areas where the existing training did not fit. For example, non-licensed staff often need to participate in code responses in ambulatory settings, there are usually a different range of emergency contact numbers needed, and, across their health system, there are six different types of automated external defibrillators (AED) machines. Nurses and staff must know how to effectively use the appropriate AED machine from their specific practice setting.
The team took an evidence-based approach to planning, by incorporating the American Heart Association's (AHA) 2020 Basic Life Support (BLS) recommendations for deliberate training with simulations. According to this research, Shorey, S., showed that virtual reality training was effective for registered nurses, and Anderson R. found skills and technique retention declined significantly after a month without practice. Regular practice is ideal for maintaining proficiency in resuscitation skills (Anderson, et al., 2019). Finally, the team drew on competencies in the Nursing Professional Development: Scope & Standards of Practice (Harper & Maloney, 2022).
Securing internal support for changing the mock code competency system was key. Nurse managers are crucial in ensuring program-wide adoption, so Bush-Foster and Duckworth actively collaborated and worked to mitigate any challenges with the proposed change to training. The Vice President of Ambulatory Nursing reviewed the program and discussed it with clinic leaders, ultimately endorsing making the new design of mock code training an annual requirement for ambulatory staff.
Delivering Effective Training: A Multi-pronged Approach
Evidence shows live, in-person training sessions are the best practice for delivering ambulatory mock code education. The new live ambulatory mock code session developed by Bush-Foster and Duckworth focuses on developing critical skills; for instance, ensuring everyone practices proper mask placement on manikins, performs effective chest compressions, and follows established rotation protocols. However, logistical limitations prevent training all 2,000 staff in the hospital system this way. To address this Bush-Foster and Duckworth developed the “Competency Champion” role and program, and, as a result, many live sessions were held in 2023.
Competency Champions attend "train-the-trainer" workshops, enabling them to deliver mock code training in their local areas and becoming subject matter experts for their colleagues. Champions are encouraged to host two in-person mock code trainings annually. Initially, champions conducted a "scavenger hunt" to identify any equipment specific to their clinic that required unique training. This approach’s success so far is evident in its growth—from 25 champions in its first year to 54 and expanding in the current year. Competency champions utilize bags filled with essential tools, such as manikins and educational resources, which they must pick up prior to training. As a way for the NPD team to ensure resource allocation, all bags are tagged with QR codes.
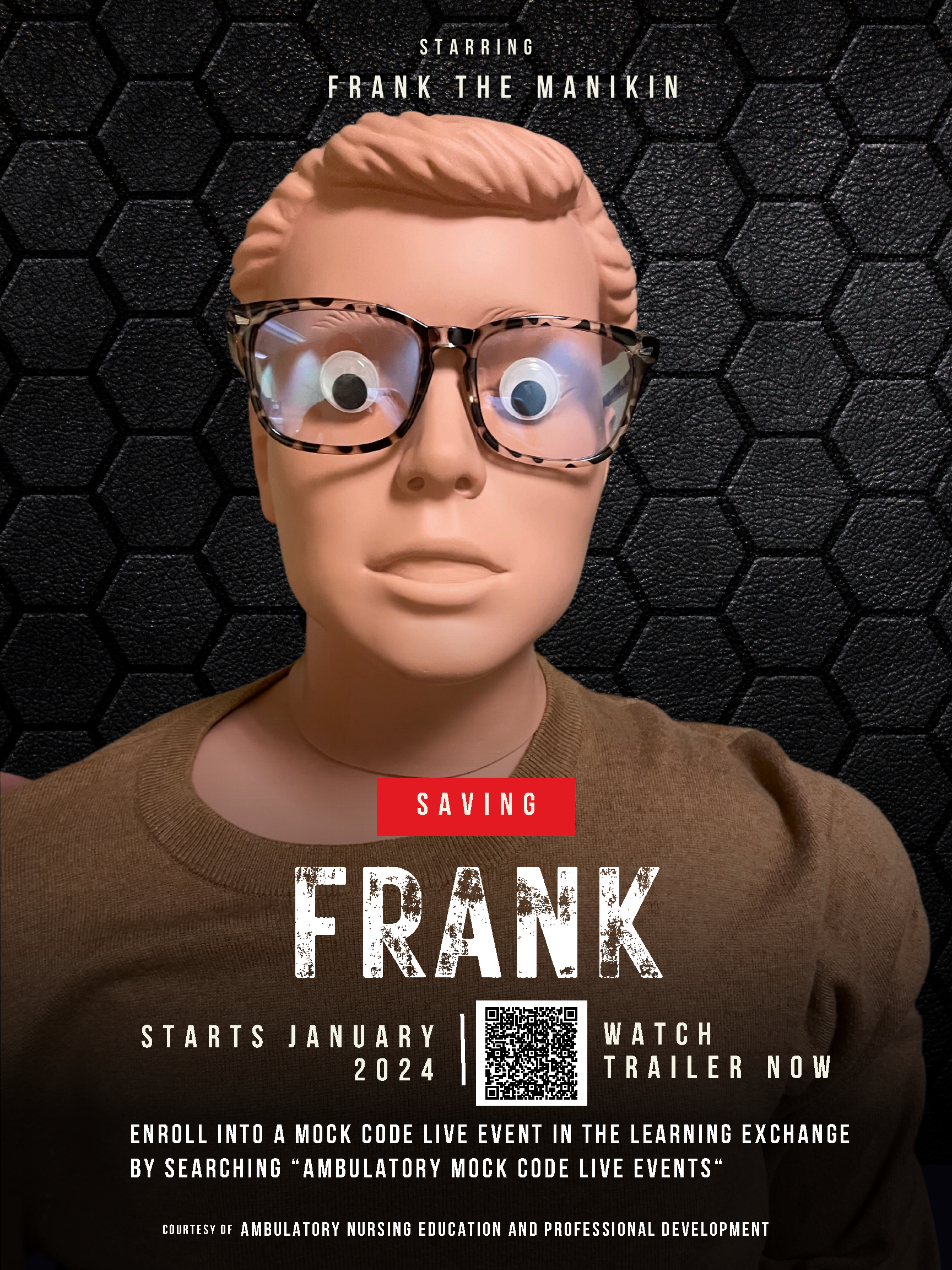 To encourage participation in live training, the team launched creative marketing campaigns. One initiative, "Mock Code Madness" held in March, generated excitement. Another campaign, "Save Frank," featured a dressed-up, googly-eyed manikin named Frank who has a cardiac arrest while being pushed into the clinic. Posters and a video trailer encouraged staff to "Save Frank" to promote the training. Nurses and staff enthusiastically responded to this lighthearted approach, often inquiring about Frank's well-being with the NPD team.
To encourage participation in live training, the team launched creative marketing campaigns. One initiative, "Mock Code Madness" held in March, generated excitement. Another campaign, "Save Frank," featured a dressed-up, googly-eyed manikin named Frank who has a cardiac arrest while being pushed into the clinic. Posters and a video trailer encouraged staff to "Save Frank" to promote the training. Nurses and staff enthusiastically responded to this lighthearted approach, often inquiring about Frank's well-being with the NPD team.
Recognizing that not everyone can attend live sessions, the NPD team also developed virtual mock code training events. These sessions utilize professionally produced videos showcasing code scenarios. To promote engagement in the digital platform, they developed two contrasting videos showcasing "bad code" and "good code" scenarios, appealing to a variety of learning styles (visual, auditory, reading/kinesthetic).
Participants interact through a chat function, identifying issues within the video and discussing best practices. Virtual training also incorporates video loops demonstrating proper hand placement for CPR and the use of various equipment found in ambulatory settings, including the six different AED models. Additionally, the virtual platform includes interactive polls to assess compression-to-ventilation ratios. To facilitate participation, all clinical workstations are equipped with Teams software, encouraging staff to turn on cameras and engage verbally. If a camera malfunctions, participation via the chat function is mandatory.
For those unable to participate in live or virtual sessions, a case study module is available within the learning management system. This interactive module includes short video clips demonstrating CPR techniques and mask placement. The module also incorporates knowledge checks with a 100% pass requirement to ensure competency.
A Successful Educational Change
The initial implementation of the new ambulatory mock code training program in 2023 yielded promising results. Over 1,150 licensed and non-licensed staff completed the training, with in-person participants reporting the highest confidence level (100%) on a post-training survey, followed closely by virtual participants (99.4%). The case study module was the most popular option, with 452 staff completing it. Based on this positive response, clinic leadership has mandated annual ambulatory mock code training for all licensed and non-licensed staff beginning in fiscal year 2024.
Bush-Foster and Duckworth acknowledge the importance of debriefing sessions following mock code scenarios to support staff well-being. They see potential for growth in expanding their competency champion network and improving equipment, as AED pads are often becoming torn and their mock code training bags are getting lost, despite their QR code tracking system.
The program's success has led to discussions about expanding code training to encompass all affiliated facilities. Real-world events highlight the need for preparedness in unexpected situations. Instances like resuscitations in parking lots, staff responding to car accidents, and overdoses left at clinic doors underscore the importance of equipping all staff with the skills necessary to handle emergencies.
By continuously evaluating and refining the program, Bush-Foster and Duckworth are ensuring that all their system staff have the knowledge, skills, and confidence to effectively manage code situations, regardless of their role or location within the organization.
An Audience Member’s Perspective
This session was a hit at the ANPD Aspire Convention, with many participants interested in implementing similar training at their health systems in the future. Colleen Coyne, RN, MSN, NPD-BC, CMSRN, was one attendee who shared her perspective and takeaways:
“It was so enriching to hear experiences from another group of ambulatory educators. In my current role, I coordinate onboarding for ambulatory nurses new to my healthcare system. This comprises 800 sites, and it can be difficult to ensure our content is applicable for every orientee we have. By sitting in on this session, I gained valuable advice on how to work on unifying my ambulatory sites.
One piece of knowledge I plan on taking back to my system is the idea of competency champions to run mock codes at the sites. I loved this idea, and I think this would empower ambulatory nurses throughout my healthcare system. A challenge to implementing this would be geographic distances. Our ambulatory sites are spread throughout a wide area—physically getting to the sites would require a lot of time and careful coordination with every site.
Overall, I loved this session. I am in the process of doing a literature review on ambulatory orientation practices, and I have found very limited amount of information available. Being able to sit in a room with and hear from other ambulatory nursing professional development practitioners was inspiring and insightful.”
References
Harper, M. G. & Maloney, P. (2022). Nursing professional development: Scope & standards of practice. The Association for Nursing Professional Development.
Shorey, S., & Ng, E. D. (2021). The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse education today, 98, 104662.
Moreno, S., Sisó-Almirall, A., Kostov, B., Expósito, M., Moreno, J. R., de Pablo, B., & Coll-Vinent, B. (2021). Cardiopulmonary resuscitation skill maintenance for primary care staff: brief training sessions with feedback. Sesiones breves con retroalimentación: una oportunidad para mantener las habilidades en reanimación cardiopulmonar en profesionales de atención primaria. Emergencias : revista de la Sociedad Espanola de Medicina de Emergencias, 33(3), 203–210.
Sydney Bush-Foster, MSN, RN, NPD-BC
Nurse Education Specialist for Adult Ambulatory, Vanderbilt University Medical Center
Sydney Bush-Foster, RN, MSN, NPD-BC, began her nursing career as a RN in surgical and cardiac units before returning to Vanderbilt University for her MSN. Afterwards, she practiced as a nurse practitioner for surgical practices at Vanderbilt for 10 years before switching to education, and she taught at the University level in BSN and collegiate RN to BSN programs. Bush-Foster also spent time in research for Vanderbilt University School of Nursing, focusing on cancer treatments and lymphedema, prior to returning to the nurse education specialist role. Her relevant teaching experience includes: BLS instructor, ACLS instructor, advanced airway instructor, and in-patient and ambulatory mock codes.

Suzanne Duckworth, MSN, RN, AMB-BC
Director of Clinical Education and Professional Development for Adult Ambulatory, Vanderbilt University Medical Center
Suzanne Duckworth, MSN, RN, AMB-BC, is the director of clinical education and professional development for adult ambulatory at Vanderbilt University Medical Center. Nursing is a second career for Duckworth, as she previously worked in the journalism space. She began her nursing career as an associate degree nurse, then obtained her bachelor’s and master’s degrees, and will graduate with her doctorate in July 2024. Duckworth worked in the NICU, adult brain injury, and with an organ procurement organization before finding her true love of ambulatory education. A diverse experience in the healthcare field has helped her understand a deeper meaning of communication and the continuous pursuit of knowledge and education. Outside of work, Duckworth enjoys running, painting, and spending time with her husband and three furry, four-legged children.