Seattle Children’s Hospital, like many hospitals across the country, has felt the sting of high nurse turnover throughout the last few years. As the hospital’s nursing professional development (NPD) team investigated the causes behind turnover, they identified a weak point: an inconsistent new nurse check-in process. As a result of these inconsistencies, it was difficult for new hires across the organization to receive the support they required. These challenges were magnified for new hires from diverse backgrounds.
Discovering how to increase staff retention is an important role of the NPD practitioner, as is the orientation and onboarding of new nurses (Harper & Maloney 2022). Seattle Children’s Hospital has historically accomplished orientation and onboarding by leveraging regular check-ins between NPDs, new hires, and preceptors to provide individualized support and to assess, define, and document goals. The NPD leadership team, including Melissa Liu, MN, RN, NPD-BC, NEA-BC, CPN, and Ashley Turner, MN, RN, NPD-BC, CPN, realized improving this process could increase retention. At the 2024 ANPD Aspire Convention, they shared their journey of discovering weaknesses within the current process, developing an approach for improvement, and implementing the new deliverables.
Investigating the New Hire Check-in Process
First, they needed to identify the key improvement opportunities within their check-in process and began with a needs assessment survey, sent to their NPD team (n=17). Results (Figures 1 – 3) were revealing:
- The use of their check-in tools varied across departments. For example, at the initial orientation meeting between NPDs and new nurse hires, some were using online forms, while others were using paper. NPDs asked different questions and documented things inconsistently, all which created barriers to effective data collection.
- Handoff between NPDs and clinical practice managers (CPMs) during escalation wasn’t always smooth. Although the organization had a documented escalation algorithm, this was not widely known to staff, was only applicable to RN residents, and was vague at times.
- Staff from diverse backgrounds reported being over-monitored as compared to peers.
Figures 1 - 3: Empowering RNs Pie Charts by ANPD
Developing an Improvement Plan
As a first step toward improvement, the NPD team created a collaborative work group with goals to identify gaps and formulate a comprehensive plan to fill them. This group comprised members from multiple departments and roles, including NPDs, clinical practice managers, and human resource consultants. The group met initially between February and April of 2022. At the meetings, they set up parameters to clarify priorities, such as implementing an electronic check-in process and standardizing communication and an escalation pathway (Figure 4).
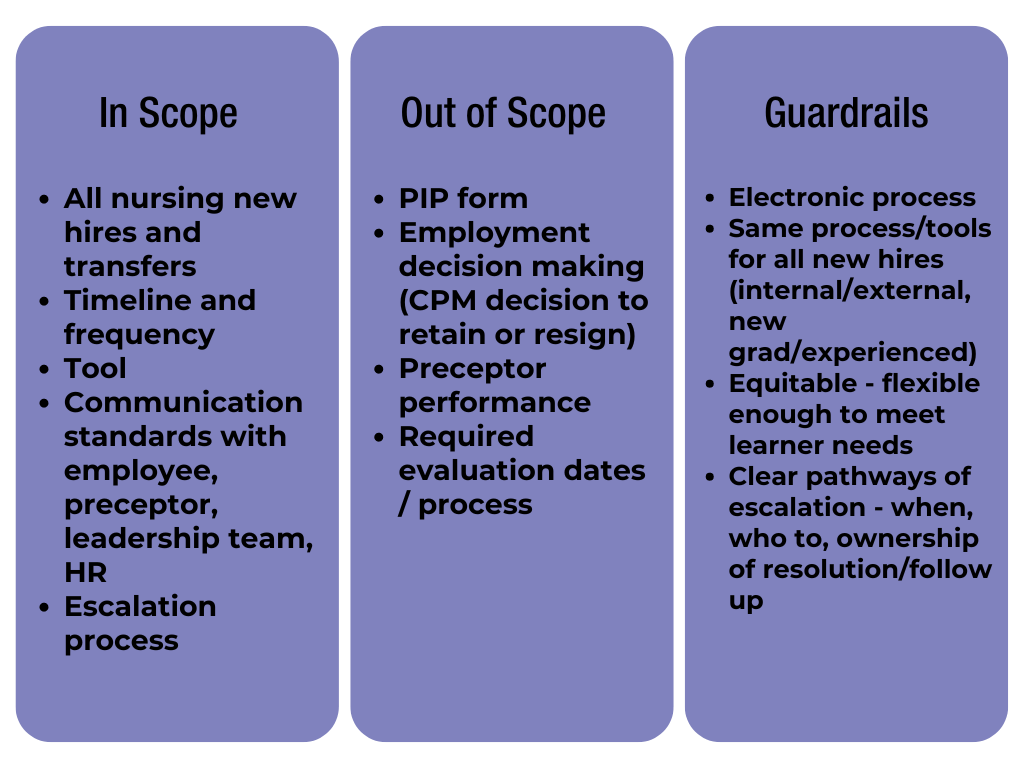
Figure 4
The group prioritized aligning their work with equity, diversity, and inclusion (EDI) values. Group members were encouraged to identify and reflect on their own implicit biases through grounding activities. These included reflecting on prompts such as "Identify a time when you were happiest: What were you doing? Who were you with? What other factors contributed to your happiness?" The grounding exercise then asks participants to identify themes in these experiences as a way to identify personal values and realize they can drive subjective biases. This approach helped lay a foundation for an inclusive environment for new hires.
The work group ended after developing three deliverables:
- A Standardized Check-in Tool and Process
The new tool is online-based and includes standard questions to review with new hires. When developing questions, they partnered with EDI leaders to ensure equitable wording. They also created a standard RN check-in form that NPDs, orientees, and preceptors would sit down together to fill out every 60 to 80 hours—usually every two to three weeks. The form includes open-ended questions centered on connecting with and understanding new staff members. The form also includes a section to document progress based on competency assessment tools grounded in the ANA Scope & Standards and encourages employees to create SMART goals that will help them continue to improve until their next check-in meeting. Halfway through these meetings, the preceptor is asked to leave to create a safe and supportive environment between the NPD and the new nurse. This check-in takes 15 to 30 minutes, depending on the needs of the orientee. A summary of each meeting is automatically sent to the NPD and CPM via Microsoft Automate.
- An Improved Escalation Pathway
In collaboration with HR partners and orientation leaders, the workgroup identified pitfalls they were seeing with current escalation processes. For example, often during the escalation process feedback given was very broad. The new escalation algorithm provided more specific paths and triggers for escalation—e.g., if an orientee was struggling with the same skill, knowledge, or behavior within a certain time frame, a clinical practice manager had to become involved. Now, we more reliably have SMART goals identified and assessed throughout the orientation process, which has allowed for quicker response and different support.
- An Emphasis on Recognizing Bias
In order to engage with the CPMs, they added a new bi-weekly meeting between CPMs and NPDs to discuss all orientees and their progress. A pause is built in at this time to ensure bias reduction—essentially, it’s a designated time for everyone to reflect on a few questions that help individuals identify any biases that may be surfacing. The intention with this was to create space to ask themselves questions that could help identify any bias, unconscious or otherwise. Questions include:
- "Is the feedback objective and observable behavior?"
- "Are there other new hires facing similar issues, and are we responding in the same way?"
- "Are there other factors at play that may be leading to the performance/behaviors that we should address?"
Starting in May 2022, a pilot with these new deliverables launched. The standard check-in process was swapped to the new version for small groups of new hires across units, and they completed 58 check-ins during the two-month pilot window. At the pilot’s end, the NPDs presented the results to the director team, clinical practice manager team, and NPD team, ensuring they addressed all questions prior to going live across the hospital.
Implementation and Results
In August 2022, house-wide implementation began, and the NPD team set an expectation of 80% compliance with the new process. In February 2023, they conducted another “Plan, Do, Check, Act” (PDCA), which resulted in a switch from Microsoft Forms to RedCap, which streamlined data collection. In addition, they added new questions about mental health support to the form, as they realized many new hires did not know about resources offered at Seattle Children’s Hospital. In October 2023, another PDCA resulted in removal of these mental health questions, as they realized responses were often vague and unactionable. Plus, their RN residency at this time had developed and implemented additional stress, anxiety, and mental health resources within the program, so the questions in the assessment became redundant. New hires who are not new graduates receive a resource review at the general orientation, and NPD practitioners have links ready to share if they express concerns or need additional support.
The visibility created through the new check-in process continued to reveal challenges related to bullying, incivility, and bias. As an effort to address these challenges, the NPD team added new questions to the check-in forms in October 2023 specifically addressing these situations, e.g., “Since our last check-in, have you witnessed any examples of bias or disruptive behavior in the workplace?” and “Are you feeling welcomed in your work environment?” and “Is there anything you feel needs to be addressed immediately?” All reports of disruptive behavior were immediately escalated to the unit director, senior director, associate chief nurse, and the chief nursing officer, who had committed to addressing these problems. During their presentation at the ANPD Aspire Convention, the Seattle Children’s Hospital NPD team shared their perspective that, although it’s easy to say, “Oh that person is just having a bad day,” about someone participating in disruptive behaviors, it’s clear these situations affect new hires and addressing them is important to improving the work environment.
A few statistics that show the results of the new processes:
- Between February 2023 and the end of 2023, 2,445 check-ins happened.
- Since October of 2023, 45 instances of disruptive behaviors were reported, all which were immediately followed up.
- Overall, the NPD team met their goal of 80% compliance to the process.
- Between August 2022 and August 2023, new hire turnover decreased by 36%, for those who had been there under a year, and it decreased by 27% for those who had been there between one and two years.
Limitations and Ongoing Work
A challenge the NPD team faces is how cumbersome it can be to review data received from the check-in forms. And because it’s manual entry, it can be difficult to achieve accuracy. For example, those filling out the forms may spell names incorrectly or use the wrong ID number.
Now, the NPD team at Seattle Children’s Hospital is implementing their new processes for new employees in other clinical roles, including to nurse techs, CNAs, medical assistants, and others, and the team is working hard to improve diversity and turnover of underrepresented new hires.
Overall, these process improvements were an NPD success. They standardized a new hire check-in process that has led to decreased turnover rates and an expectation of equitable support for all new hires. Implementing a pause for reflection on bias is another new success, and so is increasing communication between collaborative partners, improving real-time follow-up, and setting clear expectations among all team members.
References
- American Nurses Foundation. (2022, February 28). Covid-19 impact assessment survey - the second year. ANA. Retrieved February 8, 2023, from https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/covid-19-impact-assessment-survey---the-second-year/
- Gilroy, H. (2022). The Healers Are Broken: A Call for Trauma-Informed Professional Development in Nursing. Journal for Nurses in Professional Development, 38(5), 273–278. https://doi.org/10.1097/NND.0000000000000761
- Harper, M. G., & Maloney, P. (Eds.). (2022). Nursing professional development: Scope and standards of practice (4th ed.). Association for Nursing Professional Development.
- NSI Nursing Solutions, Inc. (n.d.). 2022 NSI National Health Care Retention & RN Staffing Report. Retrieved February 8, 2023, from https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf
- Reebals, C., Wood, T., & Markaki, A. (2022). Transition to practice for new nurse graduates: Barriers and mitigating strategies. Western Journal of Nursing Research, 44(4), 416–429. https://doi.org/10.1177/0193945921997925
- U.S. Bureau of Labor Statistics. (2022, September 8). Registered nurses : Occupational outlook handbook. U.S. Bureau of Labor Statistics. Retrieved February 8, 2023, from https://www.bls.gov/ooh/healthcare/registered-nurses.htm#tab-6

Melissa Liu (she/her), MN, RN, NPD-BC, NEA-BC, CPN
Director of NPD, Department of Nursing Practice, Professional Development, & Innovation, Seattle Children's Hospital
Melissa Liu is a seasoned nurse leader dedicated to enhancing nursing excellence and patient care at Seattle Children’s Hospital. With a master of nursing from the University of Washington and extensive experience spanning over a decade, Melissa currently serves as director of nursing professional development. Her role involves overseeing comprehensive programs including RN residency, onboarding, and continuing education, crucially supporting nursing staff growth and competence. Liu excels in project management and is recognized for her expertise in implementing quality improvement initiatives to elevate patient safety and operational efficiency. She actively collaborates with nursing leaders and educational institutions, fostering innovative projects that enhance clinical practice and staff retention. Liu's commitment to professional development is underscored by her certifications in nursing professional development and nurse executive leadership. Her leadership extends beyond the hospital as she engages in community service and mentors future nursing leaders through various professional associations and advisory roles.

Ashley Turner (she/her). MN, RN, NPD-BC, CPN
Nursing Professional Development Manager, Transitions in Practice & Outreach Education, Nursing Practice, Professional Development & Innovation, Seattle Children’s Hospital
Ashley Turner is nursing professional development manager at Seattle Children’s Hospital. She received her master of nursing from the University of Washington and is certified in nursing professional development. Her role involves overseeing the RN residency program, nurse technician and certified nursing assistant orientation, undergraduate nursing student clinical placements, life support classes, and the hospital's training on trauma-informed care and behavioral response. Turner has led her team through the third RN residency re-accreditation process receiving distinction through ANCC and is preparing them for their fourth redesignation. She has done extensive work to evaluate the RN residency turnover and develop initiatives and processes to improve the experience. She has been able to double the access to our undergraduate nursing students in the community through expanding access in the procedural and intensive care spaces.